As a graduate student in the field of neurodegenerative disease research, I have noticed a weight carried by my colleagues and supervisors to progress our knowledge of these devastating diseases in order to develop a cure. We are currently at a critical stage in the study of Alzheimer’s disease (AD) and related illnesses: current estimates suggest that approximately 36 million people are living with AD globally, and this figure is expected to double in the next 30 years. This is accompanied by a high financial burden, as the healthcare costs associated with AD in the United States were over $200 billion in 2014 alone. If you didn’t read my previous article on the current state of AD treatments and the outlook for the near future, here’s the summary: it’s not good.
AD is a particularly tricky disease to treat, since symptoms often only present once significant neurodegeneration has already occurred. Even when early symptoms such as changes in memory and mood are detected, a definitive diagnosis is not always possible since these symptoms are shared by many other neurological disorders. To address this challenge, the focus in the field has recently shifted towards early detection and prevention. Studies on proteins involved in the pathogenesis of the disease has led to the identification of a few key biomarkers for the early diagnosis of AD.
Amyloid-β
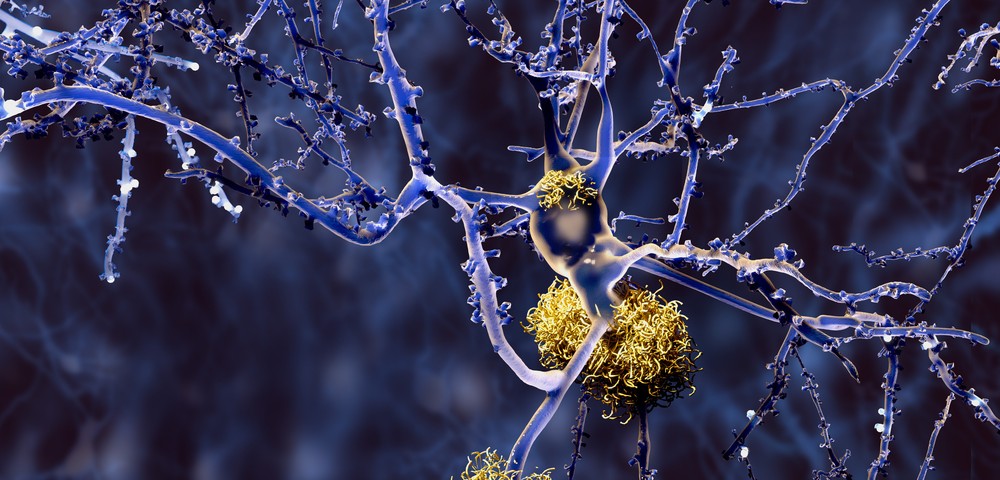
The over-production and accumulation of the amyloid-β (Aβ) peptide in the brain are thought to be the inciting events in AD pathogenesis. A 39-43-residue fragment of the amyloid precursor protein (APP), Aβ, tends to misfold, aggregate, and ultimately incorporate into the hallmark amyloid plaques seen in the brains of AD patients. The 42-residue Aβ peptide (Aβ42) is particularly toxic in AD since it's more prone to aggregation, even though it's less abundant than other variants of the peptide, such as Aβ40. By studying the biology surrounding Aβ formation and clearance, researchers have developed some useful Aβ-based biomarkers for AD.
Given that Aβ (particularly Aβ42) deposits in the brain in AD, it is reasonable to expect a reduction in this protein peripherally. Sure enough, studies evaluating the diagnostic potential of Aβ42 levels in cerebrospinal fluid (CSF) for AD observed a 50% reduction in Aβ42 compared to healthy individuals (Kapaki E et al., 2003; De Jong D et al., 2006). Similar studies investigating Aβ42 concentrations in blood plasma found that a lower Aβ42/Aβ40 ratio indicates that an individual is at risk of developing AD (Fei M et al., 2011; Chouraki V et al., 2015).
The Aβ biomarker can also be detected by direct visualization. The development of a positron emission tomography (PET) imaging agent, called Pittsburgh compound B (PiB), that binds selectively to amyloid plaques has allowed these proteins to be imaged in the brains of patients for the first time (Klunk WE et al., 2004). Previously, the presence of amyloid plaques could only be evaluated post-mortem, making this method particularly useful for the early detection of AD.
Tau
Leading theories of AD pathogenesis suggest that the accumulation of Aβ initiates a series of downstream signaling pathways that wreak havoc on another protein, tau. Tau is a microtubule-associated protein that promotes the assembly and stability of microtubules within the axons of neurons. In AD, tau becomes hyperphosphorylated, leading to the sequestration of tau itself, as well as other microtubule-associated proteins. This sequestration leads to the disassembly of microtubules, impairment of axonal transport, and eventually neuronal dysfunction. Tau hyperphosphorylation also makes the protein more likely to aggregate into long, insoluble fibers that develop into neurofibrillary tangles (NFTs), which are the second hallmark of AD pathology.
Since tau can exist in two states (phosphorylated or unphosphorylated), both states can be used as biomarkers. Compared to healthy controls, total tau levels (T-tau) in the CSF are 2-4 times higher in AD patients (Kapaki E et al., 2003; Olsson B et al., 2016). Similarly, levels of phosphorylated tau (P-tau) are also elevated by about 2-fold in patients with AD. The elevation of both T-tau and P-tau in the CSF of AD patients is thought to be a result of the degeneration of cortical neurons and axons, which release tau into the CSF when they die. Elevated Tau has even been reported in the CSF of individuals with mild cognitive impairment (MCI) who would eventually progress to develop AD, which suggests that CSF-tau might be another strong biomarker for the early stages of AD (Karch CM et al., 2012).
Neurofilament Light Protein
Unlike the previous two biomarkers, neurofilament light protein (NfL) is not a classically studied AD protein. However, in the last few years, NfL has emerged as one of the most promising new AD biomarkers. NfL is one of the three subunits which make up the neurofilament, a type of intermediate filament found only in neurons. Neurofilaments contribute to the formation of axon cytoskeletons, and when axons are compromised in AD, NfL spills into the CSF, where it can be measured to assess the degree of axonal damage. NfL levels were observed to be 2-3 times higher in the CSF of AD patients, and were also elevated in the blood plasma (Bacioglu M et al., 2016; Olsson B et al., 2016; Mattsson N et al., 2017). Since NfL is a general marker for axonal damage, it also has the potential to be used as a biomarker for other neurodegenerative diseases such as amyotrophic lateral sclerosis (ALS), Parkinson’s disease, and Huntington’s disease (Xu Z et al., 2016; Hansson O et al., 2017; Soylu-Kucharz R et al., 2017).
Other Potential Biomarkers
The AD biomarkers described above are by no means the only ones that have been investigated. Proteins such as neuron specific enolase (NSE), visinin-like protein 1 (VLP-1), chitinase-3-like protein 1 (CHI3L1/YKL-40), heart fatty acid binding protein (HFABP), and many others, have also been assessed as potential diagnostic biomarkers for AD (Olsson B et al., 2016). However, the levels of these proteins only change modestly in AD patients and therefore require larger study cohorts to be validated.
Since the ideal AD biomarker would be diagnostic for the disease, as well as provide information regarding the stage of the disease and expected rate of cognitive decline, it may be necessary to pool multiple biomarkers into a panel in order to get the full picture. This might also be accompanied by an analysis of the patients’ DNA to look for genetic changes in AD associated genes such as APP, presenilin 1 and presenilin 2 (PSEN1/2), apolipoprotein E-ε4 (APOE-ε4), and clusterin (CLU) (Huynh RA & Mohan C, 2017).
While we have much to learn about the pathogenesis and molecular mechanisms that are associated with AD in order to develop highly sensitive and specific biomarkers, we've come a long way from the rudimentary post-mortem analyses of the past century. With a number of recent philanthropic efforts underway to raise awareness and funds for AD research (such as Seth Rogen’s ‘Hilarity for Charity’ and Bill Gates’ generous $100 million donation) the future looks brighter as we continue to search for new diagnostic tools and, ultimately, a cure for AD.
Editor's note: If you are studying any of the biomarkers mentioned in this article, we put together a list of antibodies with the most published figures on BenchSci for you to review.













